INTERVENTIONS
Transcutaneous treatment of Valvular – Structural heart diseases,
Angioplasty, Treatment of Coronary Artery Disease
Transcutaneous aortic Valve replacement (TAVI or TAVR)
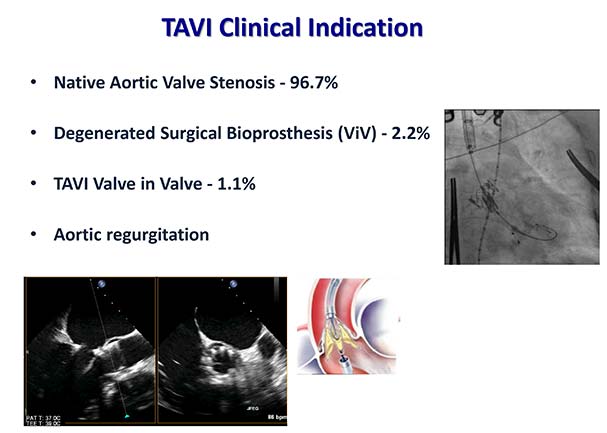
The Transcutaneous aortic Valve replacement or implantation (TAVI) is a minimal interventional procedure to replace the aortic valve in cases of severe aortic stenosis. TAVI is the method of choice in inoperable patients or patients with moderate or high surgical risk. The decision for TAVI done from our Heart Team after having a detailed medical history, clinical examination, laboratory and imaging screening of our patients.
- You have a severe aortic stenosis that causes signs and symptoms.
- Έχετε μέσο ή υψηλό κίνδυνο επιπλοκών από τη χειρουργική αντικατάσταση αορτικής βαλβίδας.
- You have an intermediate or high risk of complications from surgical aortic valve replacement. Kidney and lung disease can increase your risk of complications during surgical aortic valve replacement.
- You have an existing biological tissue valve but it isn’t working well anymore.
The risks and / or complications of TAVI are significant less compared to an open surgical aortic valve replacement. We discuss all these in a detailed fashion before the procedure.
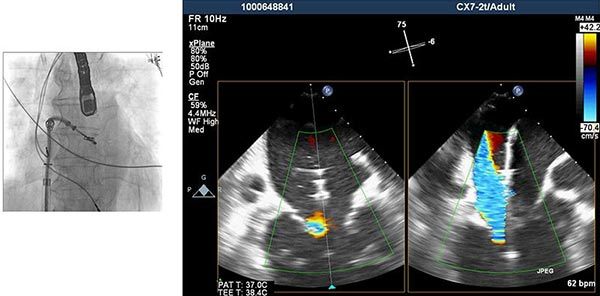
You’ll be evaluated in a detailed fashion by our Heart Team (Cardiologist, Cardiac-surgers, anesthesiologist) to make sure you don’t have any risk factors that may affect you during the procedure. Screening process is done in a regular fashion and usually includes: Echocardiography, laboratory control, MDSCT and coronarangiography. Sometimes during screening process and coronarangiography we may treat relevant stenosis in your coronary arteries. Moreover, during screening procedure we evaluate the access site, the proper device implanted and the sizing of the device.
Your treatment team will give you instructions on how to prepare for your transcatheter aortic valve replacement procedure. Talk to your doctor if you have any questions about the procedure.
The procedure is performed in our Hybrid Surgical Room with operating-room–like sterile precautions. The personnel in the room in most instances consisted of 2 interventional cardiologists, 1 cardiac surgeon, 1 cardiac anaesthesiologist, 1 cardiologist echo specialist, 2 nurses and 1 valve technician (Heart Team). All possible patient body entry sites were subjected to meticulous surgical scrubbing.
Then, you will receive sedation or general anesthesia during the TAVI procedure. A treatment team member will give you medication through an iv. to prevent blood clots.
Your treatment team will monitor your blood pressure, heart function and rhythm, and watch for any changes, which can be managed with treatments as needed during the procedure.
To perform TAVI, the doctor may access your heart through a blood vessel in your leg (like Coronary-angiography). The doctor may sometimes use other approaches to access your heart. A hollow tube (catheter) is inserted through the access point. Your doctor uses advanced imaging techniques to guide the catheter through your blood vessels, to your heart and into your aortic valve.
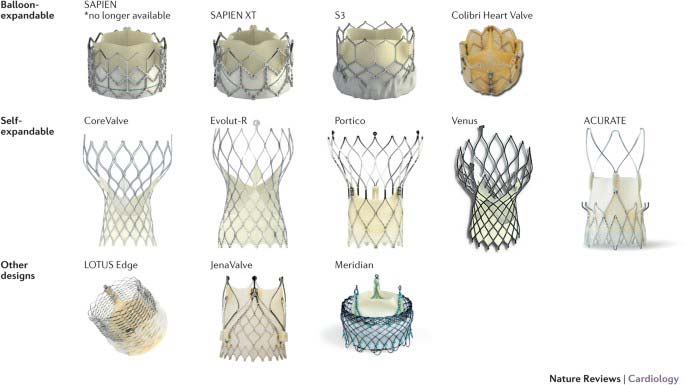
Once the new valve is positioned, a balloon on the catheter’s tip is inflated to expand the replacement valve into the appropriate position. Some valves can expand without the use of a balloon (self-expanding).
When your doctor is certain the valve is securely in place, the catheter is removed. The duration of the procedure is less than 60 minutes.
You may spend one (1) night in the intensive care unit (ICU) for monitoring after your procedure. Generally, you’ll spend about two to five days recovering in the hospital.
You’ll need regular follow-up appointments with your doctor after TAVR. Let your doctor know if you have any new or worsening signs or symptoms.
You may need to take certain medications after your procedure. For example, you’ll need to take blood-thinning medications to prevent future blood clots. Your doctor will discuss with you how long you may need to take these medications. Always take your medications as prescribed.
Artificial heart valves, including a transcatheter aortic valve, can become infected with bacteria. Most bacteria that cause heart valve infections come from the bacteria in the mouth. Excellent dental hygiene, including routine dental cleanings, can help prevent these infections. Your doctor will recommend that you take medications before certain dental procedures to prevent infections.
Your doctor may recommend that you make healthy lifestyle changes, such as eating a heart-healthy diet, exercising regularly, maintaining a healthy weight and avoiding smoking.
Transcatheter aortic valve replacement may relieve the signs and symptoms of aortic valve stenosis and improve your overall health and quality of life. Transcatheter aortic valve replacement can also reduce the risk of death.
Transcutaneouis mitral valve repair (TMVR)
Transcutaneous mitral valve repair is minimal invasive procedure for the treatment of mitral regurgitation.

TMVR should be considered:
In selected symptomatic patients with severe mitral regurgitation not eligible for surgery and fulfilling criteria suggesting an increased chance of responding to the therapy.
Candidates for this procedure are patients with:
- Moderate-severe or severe mitral regurgitation with heart failure symptoms despite the optimum medical treatment.
- Functional regurgitation (ischemic or not-ischemic) with no other indication for surgical approach.
- Degenerative mitral regurgitation deemed to be inoperable or of high surgical risk.
The risks and / or complications of TMVR are significant less compared to an open surgical approach. We discuss all these in a detailed fashion before the procedure.
You’ll be evaluated in a detailed fashion by our Heart Team (Cardiologist, Cardiac-surgers, anesthesiologist) to make sure you don’t have any risk factors that may affect you during the procedure. Screening process is done in a regular outpatient fashion and usually includes: Echocardiography, laboratory control, coronarangiography and sometimes Computer Tomography (MSCT). A very important step in this procedure is the transesophageal echocardiography to better understand the anatomy of the diseased mitral valve. Sometimes during screening process and coronarangiography we may treat relevant stenosis in your coronary arteries.
Your treatment team will give you instructions on how to prepare for your transcatheter mitral valve repair procedure. Talk to your doctor if you have any questions about the procedure.
The procedure is performed in our Hybrid Surgical Room with operating-room–like sterile precautions through your femoral vein in a manner like coronary-angiography. The personnel in the room in most instances consists of 1-2 interventional cardiologists, 1 cardiac anaesthesiologist, 1 cardiologist echo specialist, 2 nurses and 1 valve technician (Heart Team). All possible patient body entry sites are subjected to meticulous surgical scrubbing. Then, you will receive general anesthesia. A treatment team member will give you medication Intravenously (iv.) to prevent blood clots.
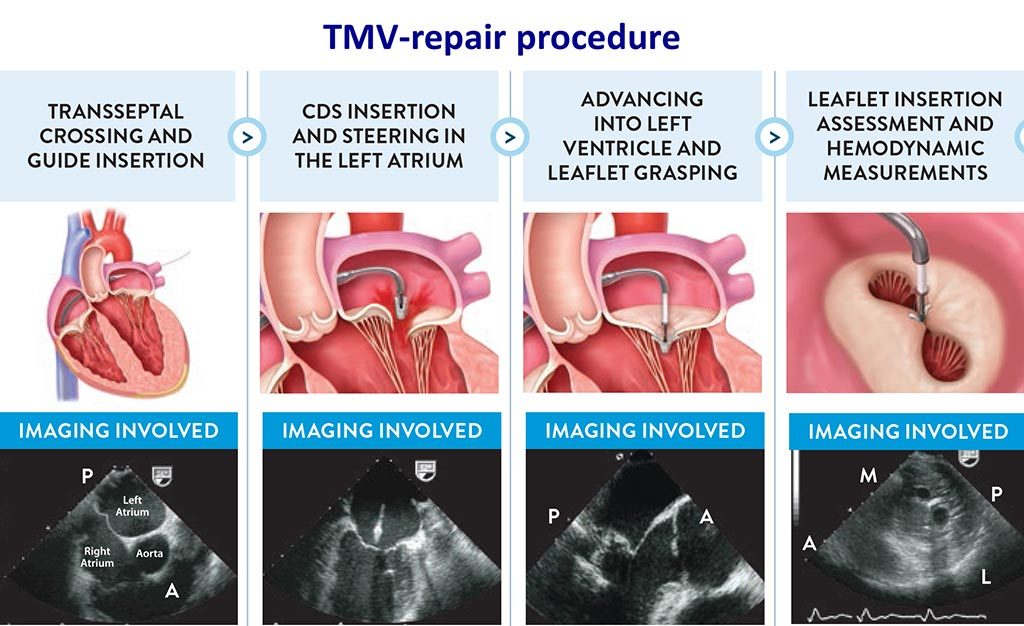
The steps of the procedure are:
- The right femoral vein was cannulated with a 7 F introducer sheath.
- Transseptal puncture 35-40 mm above the line of coaptation of the mitral valve leaflets was performed using a special needle under transesophageal echocardiography guidance.
- The Device is then advanced through the guide catheter into the left atrium, orientated appropriately over the mitral valve, advanced to the left ventricle, and then grasped. After adequate grasping of the leaflets had been confirmed, the arms were closed and the reduction in MR was assessed. We evaluate the degree of reduction, the existence of mitral stenosis and of course the efficient of grasping.
- The procedure usually last 90-120 minutes.
You may spend one (1) night in the intensive care unit (ICU) for monitoring after your procedure. Generally, you’ll spend about two to five days recovering in the hospital.
You’ll need regular follow-up appointments with your doctor after the discharge. Let your doctor know if you have any new or worsening signs or symptoms.
You may need to take certain medications after your procedure. For example, you’ll need to take blood-thinning medications to prevent future blood clots. Your doctor will discuss with you how long you may need to take these medications. Always take your medications as prescribed.
Artificial heart devices, including a those implanted during TMVR, can become infected with bacteria. Most bacteria that cause heart valve infections come from the bacteria in the mouth. Excellent dental hygiene, including routine dental cleanings, can help prevent these infections. Your doctor will recommend that you take medications before certain dental procedures to prevent infections.
Your doctor may recommend that you make healthy lifestyle changes, such as eating a heart-healthy diet, exercising regularly, maintaining a healthy weight and avoiding smoking.
Transcatheter mitral valve repair (TMVR) may relieve the signs and symptoms of mitral valve regurgitation improving your overall health, prognosis and quality of life. Several studies revealed that TMVR is safe, efficient, improves remodeling markers of left ventricle and functional capacity of patients with results remaining for at least 5 years.

Coronary Angioplasty with
Stent implantation
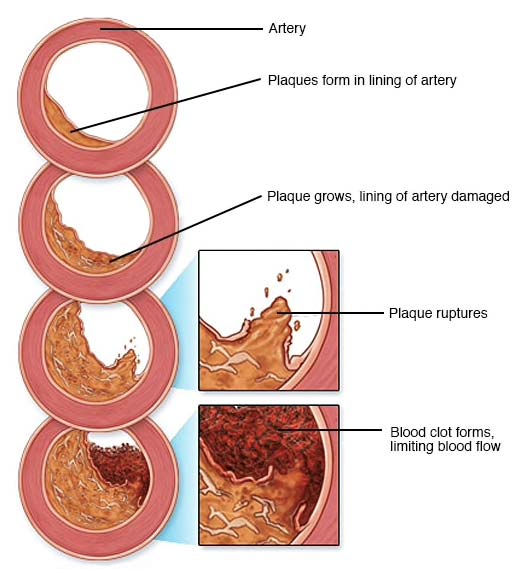
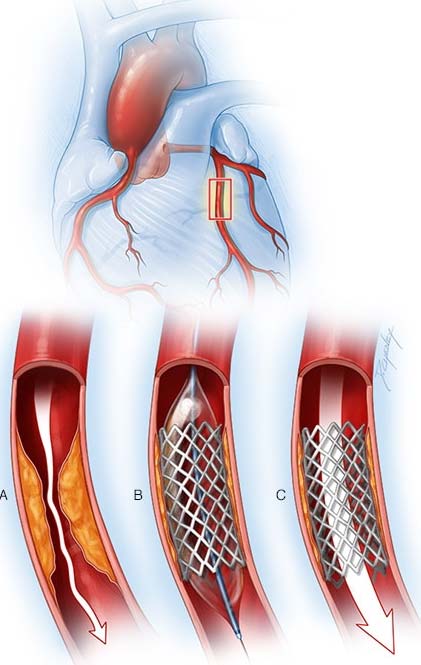
Coronary angioplasty, also called percutaneous coronary intervention (PCI), is a procedure used to open clogged heart arteries. Angioplasty uses a tiny balloon catheter that is inserted in a blocked blood vessel to help widen it improving blood flow to the heart.
Angioplasty is often combined with the placement (implantation) of a small wire mesh tube called a stent. The stent helps prop the artery open, decreasing its chance of narrowing again. Most stents are coated with medication to help keep the artery open (Drug-Eluting Stents).
Angioplasty is used to treat the atherosclerosis in the heart’s blood vessels. Angioplasty may be a treatment option for you if:
- You have tried medications or lifestyle changes but these have not improved your symptoms.
- You have chest pain (angina) that is worsening.
- You have a heart attack so called acute coronary syndrome. Angioplasty can quickly open a blocked (occluded) artery, reducing damage to your heart.
Angioplasty isn’t for everyone. Depending on the extent of your heart disease and your overall health, your doctor may determine that coronary artery bypass surgery is a better option than angioplasty for you.
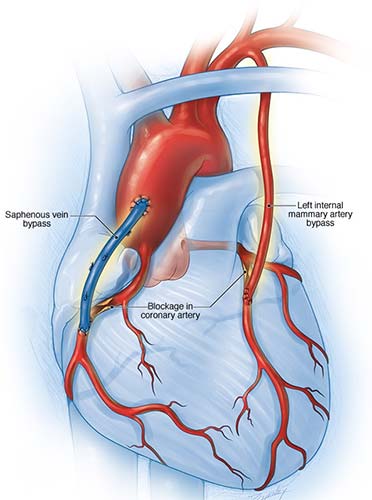
You may need coronary artery bypass surgery (CABG) if:
- The main artery that brings blood to the left side of your heart is narrow
- Your heart muscle is weak.
- You have diabetes and multiple severe blockages (multiple vessel disease) in your arteries
In coronary artery bypass surgery, the blocked part of your artery is bypassed using a healthy blood vessel from another part of your body.
Although angioplasty is a less invasive way to open clogged arteries than bypass surgery is, the procedure still carries some risks and complications. however, the risks and / or complications of angioplasty are significant less compared to an open surgery. We discuss all these in a detailed fashion before the procedure.
Before a scheduled angioplasty, your doctor will review your medical history and do a physical exam. You may need to have some tests, including a chest X-ray, electrocardiogram and blood tests, before your procedure. Your doctor will give you instructions to help you prepare.
Angioplasty is performed by a heart specialist called interventional cardiologist and a team of specialized cardiovascular nurses and technicians in a special operating room called a cardiac catheterization laboratory.
Angioplasty is performed through an artery in your groin, arm or wrist area. General anesthesia isn’t needed. You’ll receive a sedative to help you relax, but you may be awake during the procedure depending on how deeply you are sedated.
- Your heart rate, pulse, blood pressure and oxygen level will be monitored during the procedure.
- Your doctor will prepare the area in your leg, arm or wrist with an antiseptic solution and will place a sterile sheet over your body.
- Your doctor will use a local anesthetic to numb the area where a very small incision will be made. A small, thin guidewire is then inserted into the blood vessel.
- With the help of live X-rays, your doctor will thread a thin tube (catheter) through your artery.
- Contrast dye is injected through the catheter once it is in place. This allows your doctor to see the inside of your blood vessels and identify the blockage on X-ray images called angiograms.
- A small balloon with or without a stent at the tip of the catheter is inflated at the site of the blockage, widening the blocked artery. After the artery is stretched, the balloon is deflated and the catheter is removed.
- If you have several stenosis/lesions, the procedure may be repeated.
Angioplasty can take up to several hours, depending on the difficulty and number of blockages and whether any complications arise.
You might feel pressure in the area where the catheter is inserted. You may also feel some mild discomfort when the balloon is inflated and your artery is stretched, but typically you shouldn’t feel any sharp pain during the procedure.
Most people who have angioplasty also have a stent placed in their blocked artery during the same procedure. A stent, which looks like a tiny coil of wire mesh, supports the walls of your artery and helps prevent it from re-narrowing after angioplasty.
Here’s what happens during a stent placement:
- The stent, which is collapsed around a balloon at the tip of the catheter, is guided through the artery to the blockage.
- At the blockage, the balloon is inflated and the spring-like stent expands and locks into place inside the artery.
- The stent stays in the artery permanently to hold it open and improve blood flow to your heart. In some cases, more than one stent may be needed to open a blockage.
- Once the stent is in place, the balloon catheter is deflated and removed.
- More X-ray images (angiograms) are taken to see how well blood flows through your newly widened artery.
Most stents implanted during an angioplasty are drug coated. The medication in the stent is slowly released to help prevent future plaque buildup and the re-narrowing of the blood vessel.
If you had a nonemergency procedure, you’ll probably remain at the hospital overnight while your heart is monitored and your medications are adjusted. You generally should be able to return to work or your normal routine the week after angioplasty.
When you return home, drink fluids/water to help flush your body of the contrast dye. Avoid strenuous exercise and lifting heavy objects for at least a day afterward. Ask your doctor about other restrictions in activity.
Call your doctor immediately if:
- The site where your catheter was inserted starts bleeding or swelling
- You develop pain or discomfort at the site where your catheter was inserted
- You have signs of infection, such as redness, swelling, drainage or fever
- There’s a change in temperature or color of the leg or arm that was used for the procedure
- You feel faint or weak
- You develop chest pain or shortness of breath
It’s important that you closely follow your doctor’s recommendations about your treatment with blood-thinning medications — aspirin and clopidogrel (Plavix), prasugrel (Efient) or similar medications.
Most people who have undergone angioplasty with or without stent placement will need to take aspirin indefinitely. Those who have had stent placement will need a blood-thinning medication, such as clopidogrel, for six months to a year. If you have any questions or if you need any other type of surgery, talk to your cardiologist before stopping any of these medications.
Coronary angioplasty greatly increases blood flow through the previously narrowed or blocked coronary artery. Chest pain generally should decrease. You may be better able to exercise.
Having angioplasty and stenting doesn’t mean your heart disease goes away. You’ll need to continue healthy lifestyle habits and take medications as prescribed by your doctor.
If you have symptoms similar to those you had before coronary angioplasty, such as chest pain or shortness of breath, contact your doctor. If you have chest pain at rest or pain that doesn’t respond to nitroglycerin, call 911 or emergency medical help.
To keep your heart healthy after angioplasty, you should:
- Quit smoking.
- Lower your cholesterol levels.
- Eat a healthy diet that is low in saturated fat.
- Maintain a healthy weight.
- Control other conditions, such as diabetes and high blood pressure.
- Get regular exercise.
- Take medications as prescribed by your doctor.
INTERVENTIONAL REVASCULARIZATION THERAPY
Without any treatment, chronic coronary heart disease generally leads progressively to worsening of symptoms (angina), acute myocardial infarction, cardiac dysfunction and eventually death. Although some patients with coronary heart disease remain asymptomatic or show unchanged effort angina, sudden death is not entirely uncommon.
As mentioned above, the goals of treatment in chronic coronary heart disease are both the remission of symptoms and, in particular, the slowing down or halting of the progression of coronary heart disease, in order to reduce cardiovascular events and increase survival. This is usually achieved with medication, but in some cases it is necessary to achieve reperfusion (or revascularization) of the myocardium.
The therapeutic quiver currently has two major categories of invasive reperfusion methods for the treatment of patients with chronic coronary heart disease atherosclerosis: (1) the various types of transcutaneous coronary interventions, and (2) coronary artery bypass surgery.
Myocardial reperfusion is effective in relieving symptoms, but does not always increase survival. Two general categories of patients benefit in the area of survival: 1) patients with severe symptoms that are resistant to maximal medication, and 2) patients with “significant” coronary heart disease, as determined by the location and severity of atherosclerotic lesions , the number of affected coronary arteries and, finally, the presence of left ventricular systolic dysfunction.
Percutaneous coronary interventions

Percutaneous coronary interventions (PCI) include percutaneous coronary angioplasty.
Percutaneous coronary angioplasty (PTCA) consists of balloon dilation within the coronary artery stenosis and is currently the most widely used method of non-surgical reperfusion surgery. It was first applied in 1977 by Gruntzig and since then the rate of increase of its application has followed an exponential course, as the ability of the method to achieve relief of coronary symptoms was quickly realized. This significant increase in the number of performed pottery is mainly due to the improvement of the technique, the evolution of the materials used and the establishment of clear criteria for the selection of patients.
Advantages of the method are the low invasive morbidity and mortality in properly selected patients, the short duration of hospitalization and the possibility of repeated interventions, if necessary.
Disadvantages are the occurrence of restenosis even in initially successfully opened coronary arteries, and the risk of acute coronary artery occlusion or other acute vascular events during surgery, which may lead the patient to perform emergency coronary artery bypass grafting.
Significant progress in the method was the introduction of intracoronary prostheses or “stents”, which helped to reduce both the immediate occlusion and the late restenosis of the coronary arteries. Additional benefit and greater security in this direction seems to be provided by coated stents (with drugs, such as rapamycin), as they reduce the rate of hyperplasia of the inner and middle linin of the coronary arterial wall, which is a basic pathophysiological mechanism of restenosis. Finally, the introduction of newer antiplatelet drugs made a significant contribution.
The ideal candidate for PTCA and stent implantation has the following characteristics: he is a man <70 years old, has coronary heart disease with 1 or 2 atherosclerotic lesions and has an ejection fraction > 40%.
Women, elderly patients, and patients with heart failure, coronary heart disease, or recent acute coronary syndrome are more likely to have a long-term unsuccessful outcome. Patients with diabetes mellitus, multivessel disease, or renal impairment have an increased incidence of peri-invasive complications.
SUPPLEMENTARY TECHNIQUES OF TRANSCUTANEOUS
CORONARY REVASCULARIZATION
Awareness of the importance of microembolization in the distal vascular network during percutaneous coronary intervention has led to the development of devices that collect and remove microparticles of atherosclerotic plaque released during interventions.
These devices are particularly useful in thrombus-related lesions, such as venous grafts or in acute ischemic syndromes. The most well-known protection devices are the PercuSurge, Angioguard, Trap etc. catheters.
The SAFER multicenter study showed that patients who had venous graft lesions and received protection with PercuSurge during intervention had a significantly lower rate of major complications (9.6%) than those who did not receive protection (15, 6%) (p <0.008). Increased rates of cardiac enzymes and slow flow (3% vs. 9%, p = 0.02) decreased significantly. Based on this study, the use of this catheter in transdermal operations on venous grafts may be recommended.
Rotational atherectomy is based on pulverizing the atherosclerotic plaque into pieces smaller than the size of the red blood cell and removing them with the blood flow through the reticuloendothelial system. The tip of the catheter, which is olive-shaped and has tiny pieces of diamond on the front, rotates at high speeds (140,000-160,000 rpm), causing damage to calcified tissues, but not to tissues without it. Thus, the hard and calcified parts of the plaque are cut, while the softer ones are not damaged. Although the small pieces of the atherectomy are removed with the flow of blood, microembolizations can be observed, as well as an increase in cardiac enzymes by 2.5-4%.
Concomitant phenomenon, therefore, is sometimes observed slow flow or no flow peripherally, as well as activation of platelets. The method is widely used in whitewashed plates, which are believed to be difficult to open with the balloon, in order to facilitate stent placement.
The microtome balloon, as the cutting balloon can be, is a modification of the classic pottery balloon, on the surface of which 3 isosceles micro-blades have been adapted which, in the full development of the balloon, protrude 0.25 mm. The blades aim to achieve controlled separation of the atherosclerotic plaque during dilation, thus avoiding extensive separations, less injury to the vascular wall, and less elastic restoration of the vessel.
It seems that the use of the balloon is accompanied by somewhat better results than the simple pottery balloon. It seems to be particularly helpful in better restorative drilling within the stent, due to its ability to remain stable in the position it is placed in and not move during balloon dilation outside the stent.
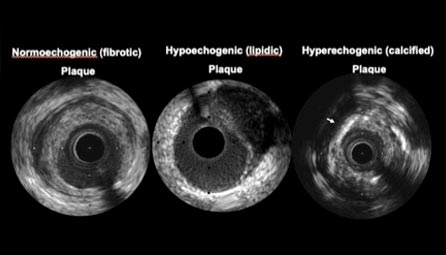
With intracoronary ultrasound it is possible to internally visualize sections of the coronary artery and obtain information about the exact dimensions of the lumen, intermediate stenoses, the condition of the vascular wall and the composition of the atherosclerotic plaque, which are impossible to identify with other imaging techniques. Intracoronary ultrasound has significantly contributed to the understanding of the mechanisms of action of angioplasty.
Thus, information related to the composition of the atherosclerotic plaque helps in the best choice of the type of invasive technique, but also in the correct choice of dimensions of stents. There is currently evidence from studies showing that the use of intracoronary ultrasound can improve the development of stents, even if they appear angiographically to have ideal growth.
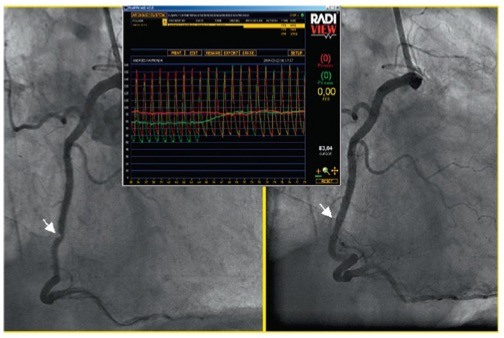
Intracoronary pressure gradient before and after stenosis was initially used to assess the results of angioplasty. Fractional coronary reserve is the ratio of post-stenotic coronary pressure to aortic pressure in a state of maximal hyperemia. The normal value is independent of : hemodynamic status and microcirculation.
The FFR is easier to calculate than the CVR, as it does not require reference artery measurements. Values less than 0.75 are equivalent to a positive ischemia test, while FFR values greater than 0.9 are equivalent to very good balloon angioplasty results, and an FFR value greater than 0.94 is equivalent to an ideal stent development.
Optical coherence tomography (OCT) is a light-based imaging modality which shows tremendous potential in the setting of coronary imaging. OCT has the ability to characterize the structure and extent of coronary artery disease in unprecedented detail as the various components of atherosclerotic plaques have different optical properties. Typically, calcified, fibrous and lipid-rich plaque components can be distinguished.
These diagnostic capabilities are being applied to study patients with acute coronary syndrome in order to improve our understanding of the pathophysiology and progression of atherosclerosis.
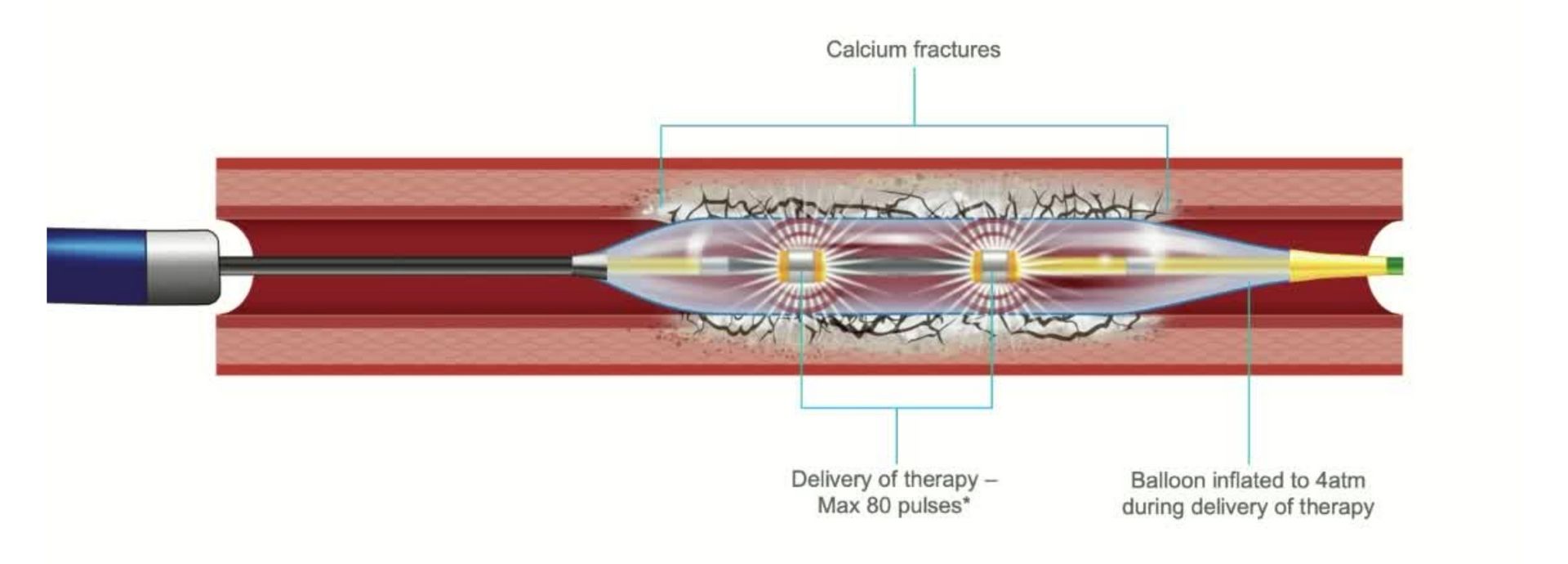
Intracoronary Lithotripsy (IVL) is a novel tool than can be used for preparation in calcified coronary artery lesions prior to stent implantation. IVL creates calcium microfractures, enhancing vessel compliance and allowing adequate dilatation of calcified lesions. IVL has FDA approved for coronary use in 2021. Unlike other technologies it’s use is very similar to conventional PCI making it relatively easy to learn and implement. Recent data (DISRUPT CAD trials) has confirmed IVL as a safe tool with high procedural effectiveness and low rates of procedural complications in patients with stable coronary artery disease as well as acute coronary syndrome, including myocardial infarction.